How does it help to predict upper limb motor outcomes?
Being able to predict upper limb motor outcomes for individual patients soon after stroke could help in several ways. For example, knowing the level of predicted motor recovery could help with discharge planning and realistic goal setting for clinicians and patients. It could also help with the appropriate allocation of time and resources by both the patient and the therapy team.
Clinicians often find it difficult to accurately predict functional outcomes, especially for patients with moderate to severe initial impairment. Currently, no single clinical measure or neurological biomarker is able to accurately predict motor recovery or outcome for all patients. Approaches using combinations of measures and biomarkers are needed.
What did the original PREP prediction tool look like?
The original PREP prediction tool combined clinical measures and neurological biomarkers in the initial days after stroke to predict upper limb functional outcomes at 3 months. It included a shoulder abduction and finger extension (SAFE) clinical score, transcranial magnetic stimulation (TMS) to assess corticospinal tract function and magnetic resonance imaging (MRI) to evaluate the structural characteristics of white matter in the posterior limbs of the internal capsules. Each of these was not required for all patients though, for example a SAFE score alone allowed a prediction for almost 50% of patients.
The original PREP prediction tool was developed in a sample of 40 patients and validated in a sample of 192 patients. Using the prediction tool in clinical practice increased therapist confidence, modified therapy content, and was associated with a 1 week reduction in length of stay, with no detrimental effects on patient outcomes.
The main strength of the original PREP prediction tool was that it was a simple, sequential decision tree. Its limitations include predicting the minimum level of function that the patient could be expected to achieve within 3 months, rather than a specific level of function which would be more useful. It also required TMS and MRI for some patients which many clinical settings do not have the equipment or expertise to perform.
What does the PREP2 prediction tool look like?
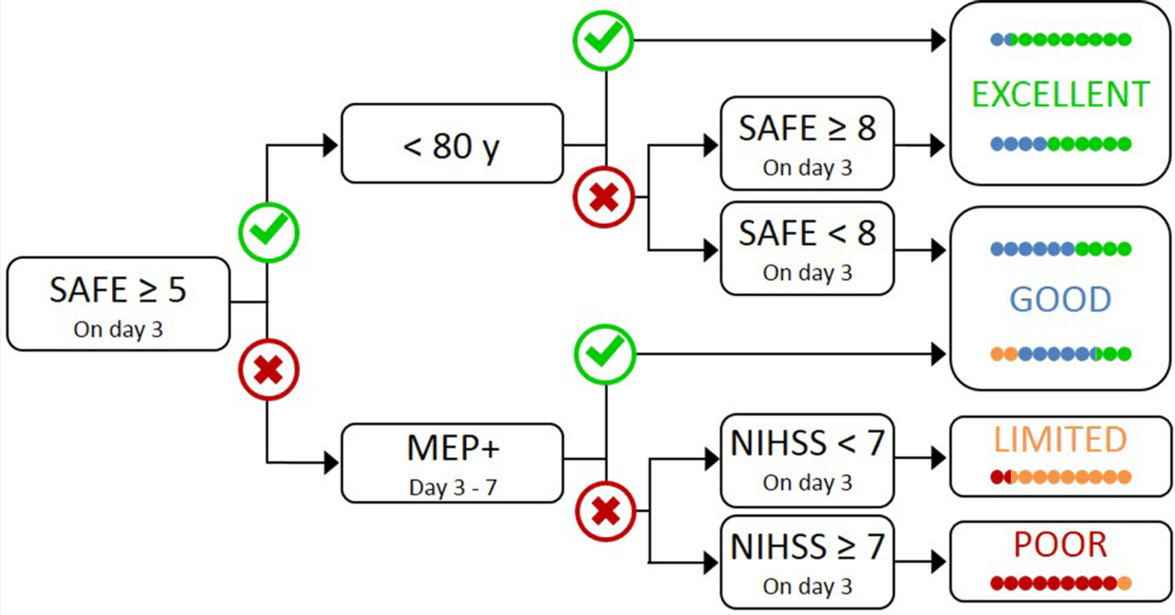
PREP2 is a modified and improved version of the original PREP prediction tool that predicts an Excellent, Good, Limited or Poor upper limb motor function outcome for individual patients. If a patient achieves a SAFE score of five or more within 72 hours post-stroke, knowing their age allows prediction of an Excellent or Good upper limb outcome. If the SAFE score is less than five at 72 hours post-stroke, the NIHSS score can be obtained at this time and a TMS assessment scheduled within the next 3 days. Patients in whom TMS elicited MEPs in the paretic upper limb (MEP+) are predicted to have a Good outcome. MEP- patients with an NIHSS score <7 are predicted to have a Limited outcome, while MEP- patients with an NIHSS score ≥7 are predicted to have a Poor outcome.
How well does PREP2 predict upper limb outcomes?
PREP2 was developed in a study including 207 stroke patients recruited within three days post-stroke. Overall, PREP2 correctly predicted upper limb outcome for 156 of 207 patients (75%). Of the remaining 51 patients, the prediction tool was too optimistic for 35 patients and too pessimistic for 16 patients. Most of the patients for whom the prediction tool was too optimistic were predicted to have an Excellent outcome, but had a Good (n = 25) or Limited (n = 1) outcome instead. Almost all of the patients for whom the prediction tool was too pessimistic were predicted to have a Good outcome, but had an Excellent outcome instead (n = 14).
Combining a patient’s SAFE score with their age was able to provide a prediction for 68% of patients and discriminate with 78% accuracy between patients who had Excellent or Good upper limb function 3 months post-stroke. For patients with a SAFE score below 5, NIHSS score without MEP status was only able to accurately predict either a Good or Poor outcome with 55% accuracy. The addition of TMS biomarker information increased prediction accuracy to 70% for these patients, highlighting the importance of testing corticospinal tract function in patients with more severe motor impairment.
How is PREP2 better than the original PREP prediction tool?
PREP2 addresses some of the limitations of the original PREP prediction tool. Efficiency was improved by the finding that patients with a SAFE score of five or more are MEP+. This means that TMS is only required for a third of patients using PREP2, instead of more than half if using the PREP prediction tool. Accessibility is improved by replacing MRI scans with NIHSS score 3 days post-stroke, which can be used with equivalent accuracy.
Despite these simplifications, PREP2 correctly predicts the actual upper limb functional outcome for 75% of patients, which is an improvement on the 64% accuracy of the original PREP prediction tool. Predictions were too optimistic for most of the remaining 25% of patients and erring on the side of optimism is preferable to the alternative, to avoid reducing patient and therapist motivation. The outcomes “complete” and “notable” in the original PREP prediction tool have also been renamed to Excellent and Good, respectively.
What are the limitations of PREP2?
One of the limitations of PREP2 is that the study that developed it included a small number of MEP- patients relative to MEP+, and patients with previous stroke or intracerebral haemorrhage were relatively under-represented. Another limitation is that PREP2 requires TMS for a small proportion of patients and there are barriers to using this technique in a clinical setting. The major barrier is the cost of the TMS equipment but this might be offset by a reduced average length of stay when PREP2 predictions are used in clinical practice.
What is the next step for PREP2?
PREP2 remains to be validated in other clinical environments, and a multi-centre trial could be performed in order to achieve this. Other possible predictors of upper limb outcome also need to be explored, such as impaired upper limb somatosensation, vision, visuospatial attention, and cognition. It is possible that PREP2 predictions, which are based on motor system measures, are less likely to be achieved when the patient’s motor performance is also affected by deficits in sensory and cognitive domains.
Further work could usefully explore other neuroimaging biomarkers that might provide important prognostic information for MEP- patients. These may involve measures of alternative descending motor pathways, and of the wider ipsilesional and contralesional sensorimotor networks, including the corpus callosum. However, more sophisticated measures may also require expertise not readily available in most clinical settings.