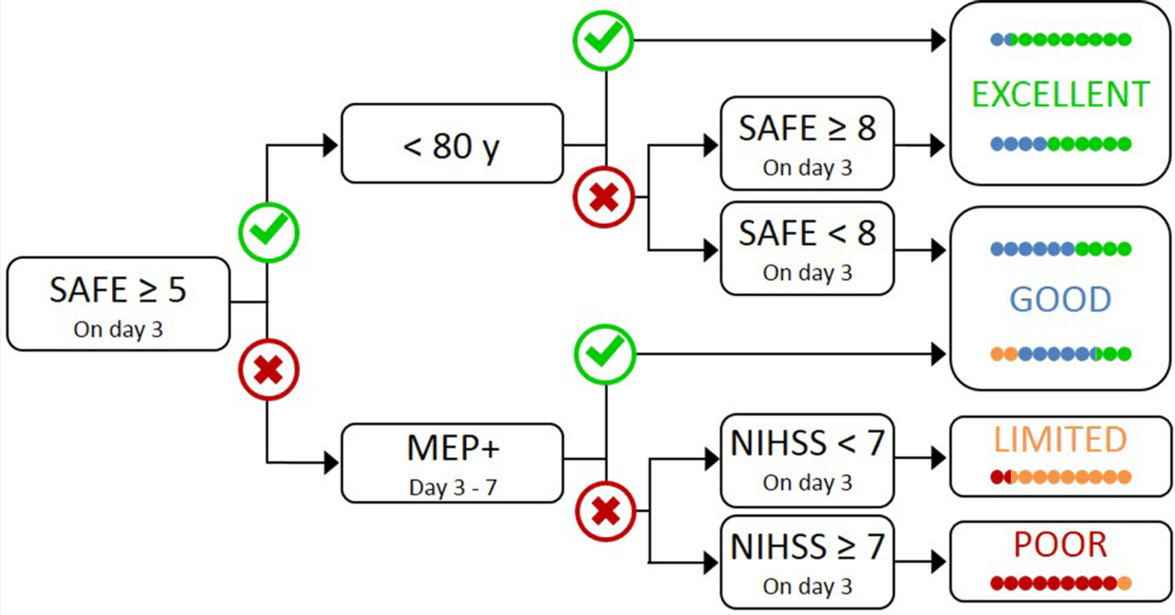
PREP2 predicts a patient’s likely upper limb functional outcome after stroke. PREP2 is started within 3 days after a stroke and is a sequence of 3 tests. The first test is all that’s required for approximately two-thirds of patients. Upper limb function at 12 weeks after stroke is predicted to be Excellent, Good, Limited or Poor.
This page provides information about each step of the PREP2 prediction tool and how it can be used to tailor upper limb rehabilitation.
You can download, share and cite a PREP2 prediction tool overview here.
Who is PREP2 for?
- PREP2 is designed for patients who are older than 18 years and have had a recent stroke (excluding cerebellar stroke) that has caused weakness in the hand and arm.
- PREP2 can be used with patients who have had an ischaemic or haemorraghic stroke, and patients with previous stroke.
- PREP2 may not be suitable for patients who have severe aphasia or cognitive impairment that limits their ability to understand the tests involved, or if there are contraindications to TMS.
PREP2: A three step process
Step 1
The first step of PREP2 is to establish a patient’s SAFE score within 72 hours of stroke. The SAFE score is calculated by scoring Shoulder Abduction and Finger Extension separately, using the Medical Research Council grades. The patient’s strength in each of these movements is scored between 0 and 5, where 0 is no muscle activity and 5 is normal strength and range of movement.
You can use the grades below, and avoid using + and – signs to keep things simple.
0 = no palpable muscle activity
1 = palpable muscle activity, but no movement
2 = limited range of motion without gravity
3 = full range of motion against gravity, but not resistance
4 = full range of motion against gravity and resistance, but weaker than the other side
5 = normal power
Shoulder abduction should be tested with a long lever, resistance applied proximal to the elbow and taken through a full range of motion. Finger extension should be tested with the wrist stabilised, resistance applied distal to metacarpal phalangeal (MCP) joints and taken through a full range of motion.
If the fingers have unequal strength, use a majority rule. If three fingers have the same score, use this score. If two fingers have a lower score than the other two fingers, use the lower score. For patients with inattention or fatigue, effort needs to be made to ensure the patient is focused on the arm to give the most accurate indication of strength.
The scores for shoulder abduction and finger extension are added to form the SAFE score out of 10. If the SAFE score is 5 or more, no further tests are required.
- If the patient’s SAFE score is ≥ 5 and they are less than 80 years old, they are most likely to have an Excellent functional outcome for their upper limb.
- If the SAFE score is ≥ 5 and they are 80 or more years old, their SAFE score needs to be at least 8 to have an Excellent prognosis, otherwise they are most likely to have a Good functional outcome for their upper limb.
- If the SAFE score is < 5, TMS assessment is required before a prediction can be made.
So far, we have found that a prediction can be made for around two thirds of patients using just their SAFE score and age.
Step 2
The second step of PREP2 is to test the function of motor pathways between the stroke-affected side of the brain and the affected hand and arm using TMS (Transcranial Magnetic Stimulation). This is a non-invasive test that takes about 20 minutes and can be done at the patient’s bedside. A safety screening questionnaire and a detailed TMS protocol are available to download from the Resources page.
The TMS assessment is carried out 3 – 7 days after stroke. If TMS produces detectable responses (motor evoked potentials, MEP+), then the patient has potential for a Good functional outcome for the upper limb. So far, we have found that about half of patients can be classified after the TMS step.
If TMS does not produce detectable responses (MEP-), then the third step of PREP2 is needed.
Step 3
The third step of PREP2 uses the patient’s NIHSS score (National Institutes of Health Stroke Scale). This score is obtained 3 days after stroke for all patients with a SAFE score < 5, in case they turn out to be MEP- and proceed to this final step. You can complete online training and certification in using the NIHSS here, by registering, logging in, and then clicking on ‘My Activities’.
The NIHSS provides a measure of stroke severity, with higher scores indicating greater stroke severity.
- If the patient’s NIHSS score is < 7, they are most likely to have a Limited functional outcome for the upper limb.
- If the patient’s NIHSS score is ≥ 7, they are most likely to have a Poor functional outcome for the upper limb.